‘Top 10 Ways to Boost Your Immune System’
If you see any rendition of these words – run.
The prevalence of “health fraud” has increased drastically since the start of the COVID pandemic, with companies receiving warnings for issuing statements and claims unsupported by science and misleading, especially in the nutrition and supplement sector (list of companies who were issued warnings located here).
There are dietary strategies and supplementation that can support immunity.
Our immune system is a multi-layered defense system. On the frontline are our physical barriers such as our skin, mouth, eyes, and gastrointestinal tract. These physical barriers are then followed by the inflammatory response – think hand-to-hand combat – and make up our innate immunity. Next is our highly-specialized forces equipped with the necessary weaponry to target specific threats – our acquired immunity.
These branches of our innate and acquired immune system work together to resist infection and illness; however, a recent publication by Neil Walsh has introduced the concept of ‘tolerance’ and also provides the basis for the nutrition strategies that support our immune system.
Calling to action all branches of your immune system is very costly – think high energy or caloric needs, redirect resources away from vital functions, and damage tissues that can occur. Not every threat requires a full-scale response and can be, well, tolerated. Tolerance is the ability to control infection at a non-damaging level. (1)
When it comes to nutrition, deficiencies in energy and nutrient intake can impair immune resistance and increase illness risk. There are specific nutrition strategies that can enhance our ‘tolerance’, often reducing the incidence, shortening the duration, and decreasing the severity of symptoms. (1)
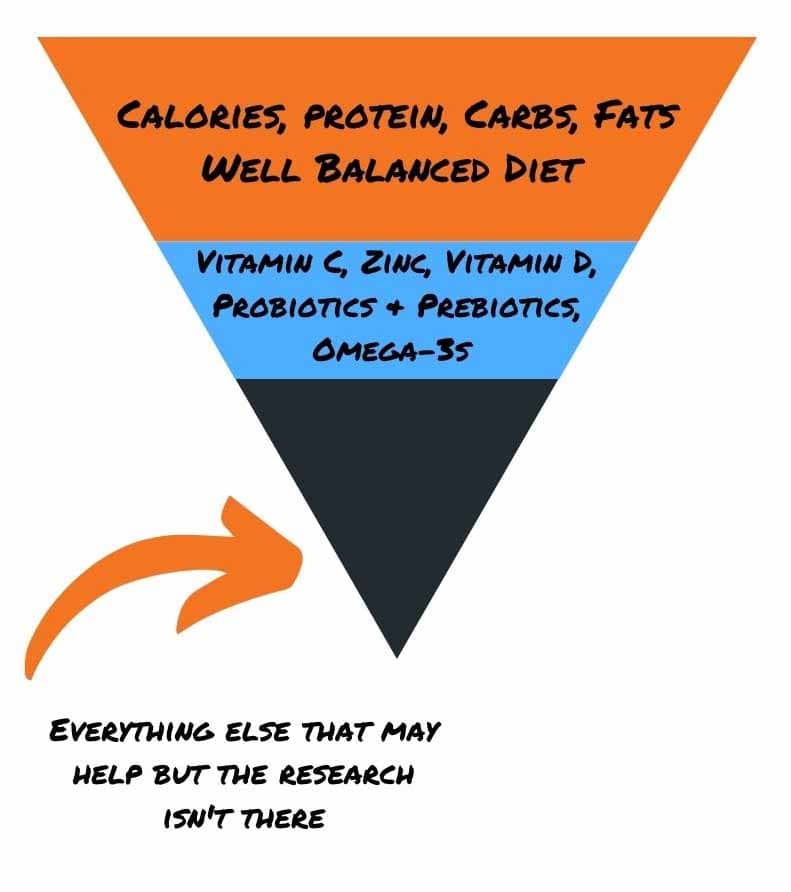
Nutrition to Support Immune Function
Adequate Calorie and Macronutrient Intake
Your immune system’s overall ability, the clearing of viruses and bacteria from the body, depends on adequate availability of energy (calories) and adequate intake of carbohydrates, protein, and fats.
We see an increase in stress hormone levels during severe caloric-protein restriction, and the overall immune response is impaired. Athletes in low energy availability (LEA) state are 50% more likely to experience upper respiratory tract infections (URTI). (2,3)
Protein plays an essential role in providing the amino acids necessary for DNA and RNA synthesis, protein synthesis, and the production of proteins such as immunoglobins and cytokines – our immune weaponry. Inadequate protein intake can increase susceptibility to infection in athletes. (1)
After training sessions with a high level of exertion or during periods of heavy training, the immune system gets suppressed, and stress hormones, such as cortisol, become elevated. This mix of stress and intensity is associated with an increased risk of infection, especially URTI. (4)
Suboptimal intake of carbohydrates is related to elevated stress hormone levels and further suppression of the immune system. Consuming adequate carbohydrate provides the necessary fuel for the immune system to run. Consumption of 30-60 g of carbohydrate during a prolonged training session can aid in maintaining a normal immune and stress hormone response after training. Therefore, proper carbohydrate consumption can minimize the “open window” or the risk of infection during heavy training periods or sessions. (5)

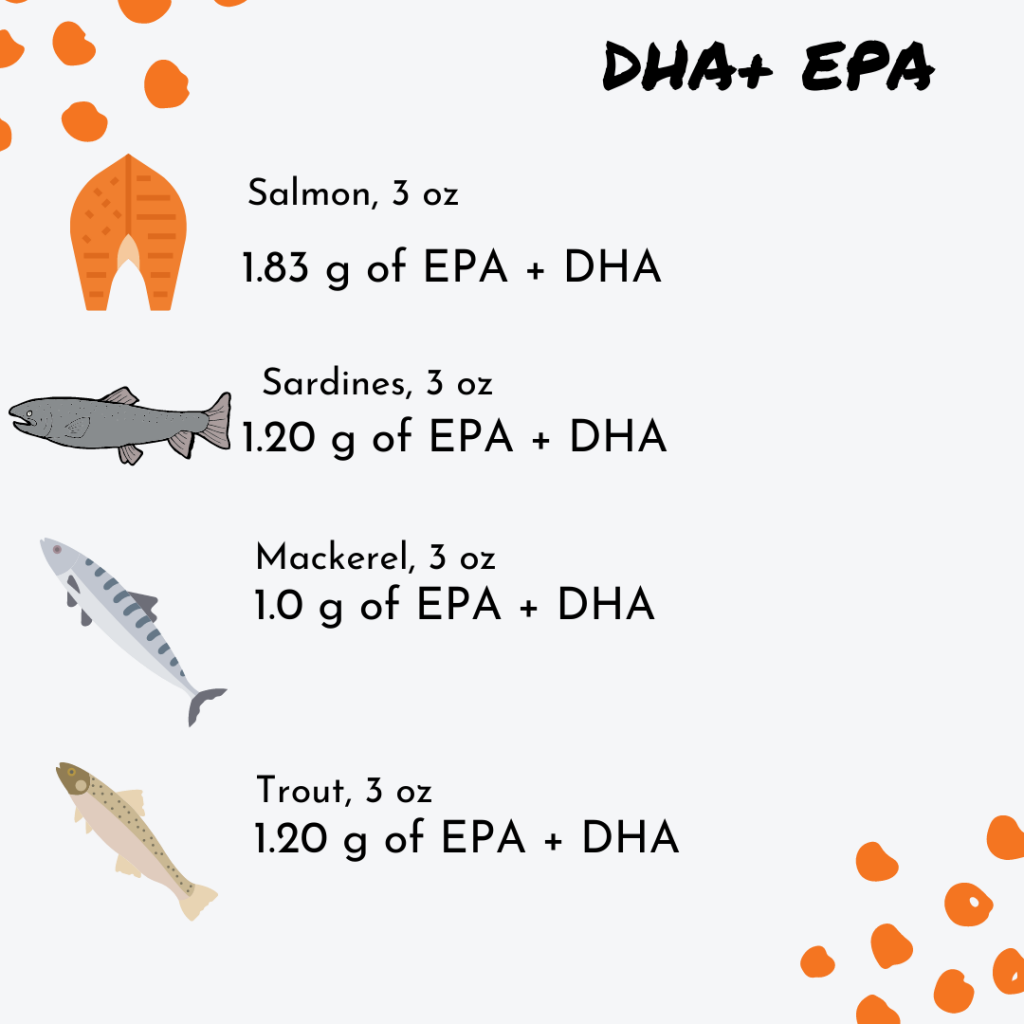
Dietary fats, specifically omega-3s, found in cold-water fish, play a role in maintaining the intestinal (gut) barrier and influence immune function through the inflammatory process. (1)
The essential omega-3s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) serve as an anti-inflammatory. Furthermore, these essential omegas provide neuroprotective benefits (check out this article on omega-3s and concussions in athletes), and necessary for overall health. (1)
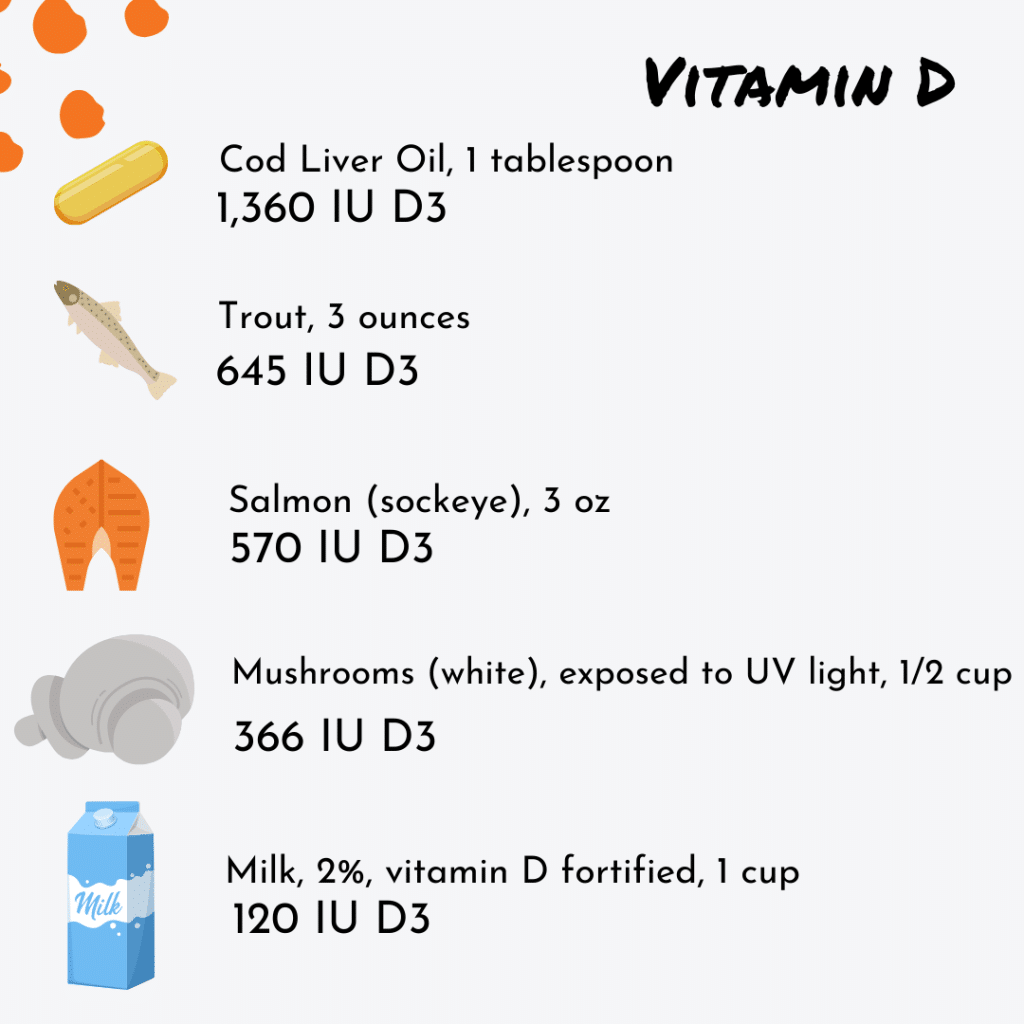
Vitamin D
Known as the sunshine vitamin and most often associated with bone health, Vitamin D also plays a role in immune function. Vitamin D deficiency can hurt immune health and possibly muscle health. (1,6)
There are vitamin D receptors located on immune cells. Vitamin D can directly influence our tolerance by enhancing immune cell activity, decreasing inflammation, and increasing anti-microbial agents. (1)
Vitamin D insufficiency is most prevalent during the winter months, and supplementation in athletes has shown to reduce URTI risk. (1,7,8)
Additionally, athletes who participate in indoor training and sports are more likely to have deficient or insufficient circulating vitamin D levels, requiring higher supplementation levels.
When it comes to vitamin D intake, more is not better. Avoid mega-dosing. Daily intake of vitamin D can range from 1,000-4,000 IU of D3 daily for athletes. (1,7,8)
Probiotics
We are finding out that our gut plays a much larger role in our health outside of digestion and absorption. It can communicate with your brain, regulates appetite, and plays a role in immunity. Your GI tract is firstly considered a physical barrier and part of that first line of defense of your immune system.
Probiotics, the beneficial bacteria that reside in the gastrointestinal tract and that make up your gut microbiota, can reinforce the gut barrier (provide extra-protection), crowd out the harmful bacteria, and influence the inflammatory response (shorten the duration). (1)
Probiotic-containing foods include:
- Yogurt, kefir
- Sauerkraut, pickles, kimchi (need to be refrigerated in stores, not heated to high temperatures as that kills the probiotics)
- Tempeh and miso

Supplementation with probiotics has shown to influence your microbiota and may reduce URTI incidence by 50% and shortened the duration of a URTI by ~2 days (9). A study looking at elite distance runners showed a reduced URTI duration and severity of URTI symptoms after 28 days of probiotic supplementation (10).
Vitamin C
Vitamin C is an antioxidant found in high concentrations in white blood cells.
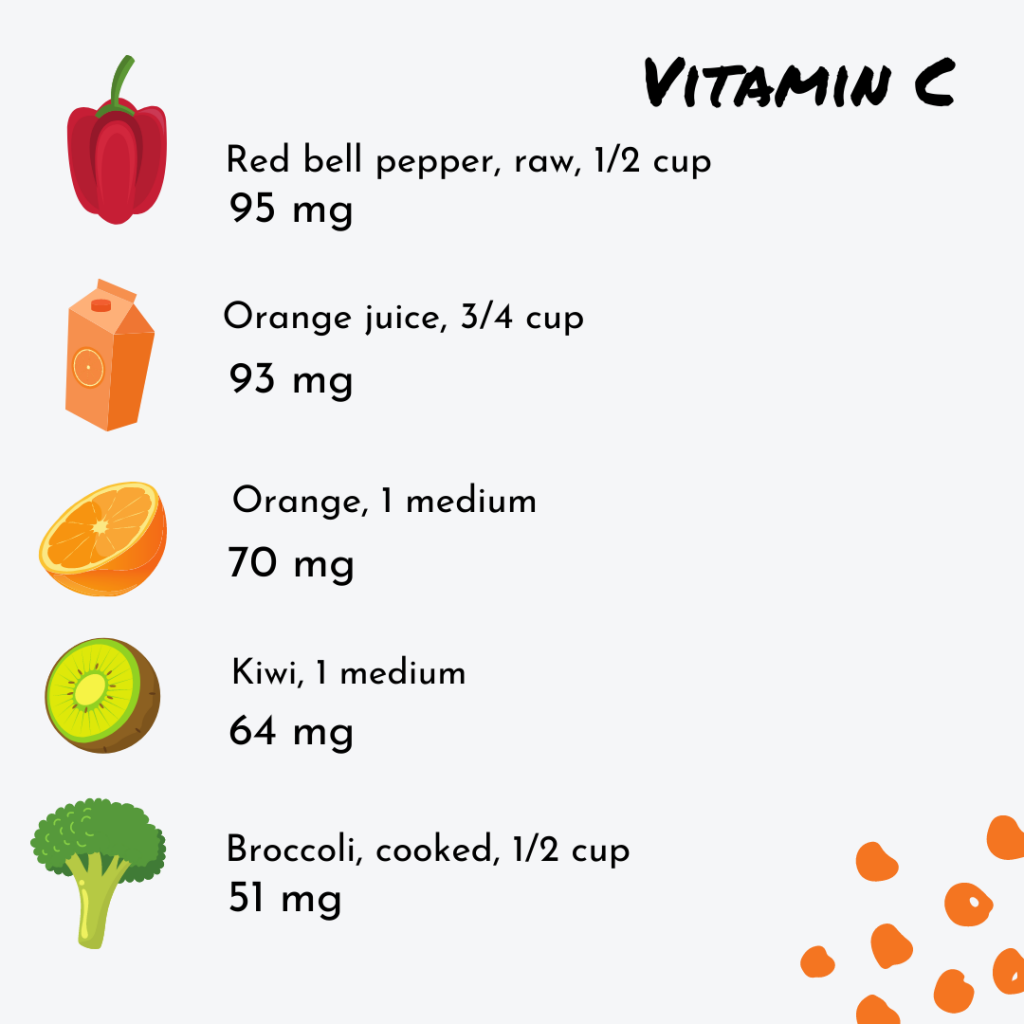
The daily recommended intake of vitamin C for 14-18-year-old males and females is 75 mg and 65 mg, respectively, and 90 mg and 75 mg for males and females 19 years and older.
When infected with the common cold, vitamin C levels fall, and vitamin C intake requirements increase to 100-200 mg per day and possibly more. It is important to note that higher amounts of vitamin C depend on the disease state or whether you are sick or not. Mega-dosing is not necessary nor recommended unless medically indicated. (1,11)
To put 100-200 mg in perspective of food, 1/2 up of red bell pepper contains 95 mg of vitamin C and 3/4 cup of 100% orange juice contains 93 mg. Hitting that 100-200 mg of vitamin C can easily be obtained through food.
Iron & Zinc
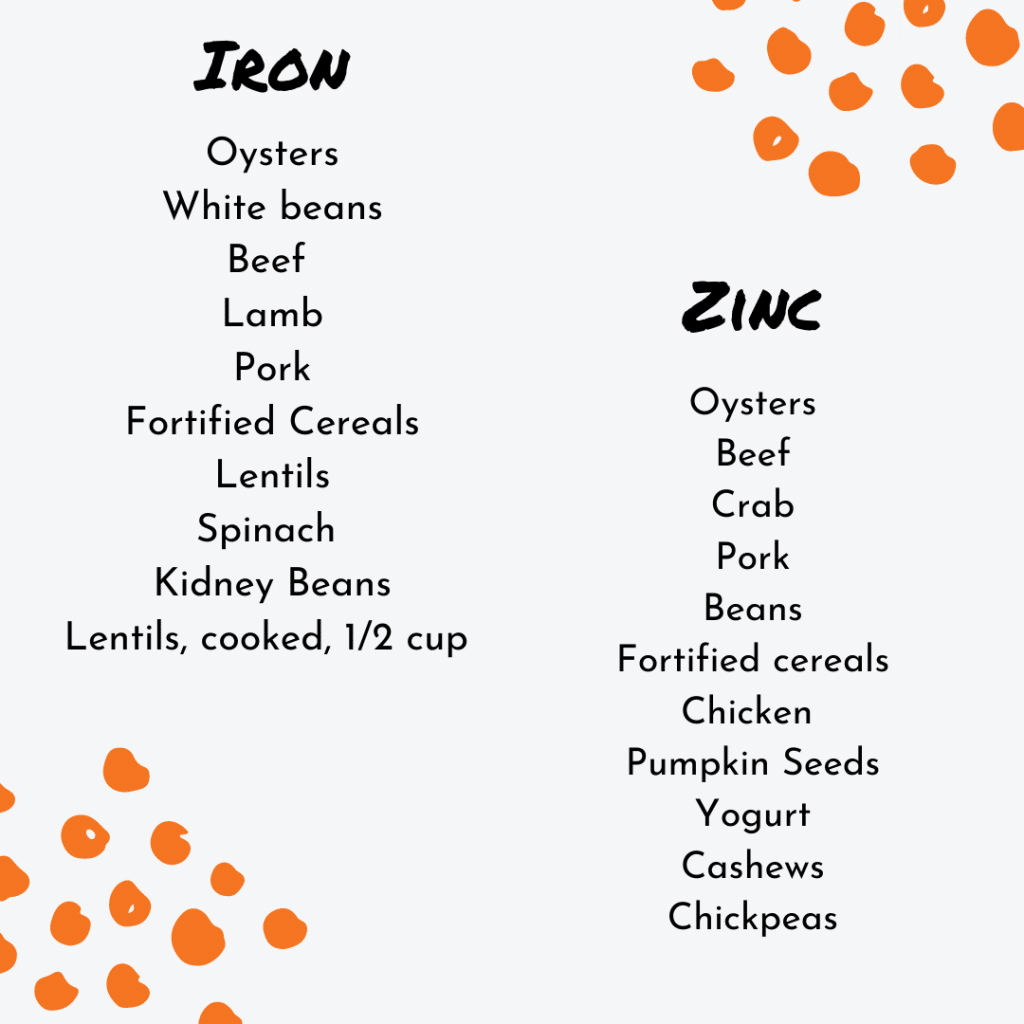
Iron is fundamental in the immune system and is essential in the immune response. (1)
Zinc, another mineral, plays a critical role in immune health, protein synthesis, and DNA and RNA synthesis and can function as an antioxidant and exert anti-inflammatory effects. (1)
Zinc lozenges, containing 75 mg of elemental zinc per day, reduced URTI duration by ~3 days when taken within the first 24 hours after the onset of symptoms (12). There is no evidence to support prophylactic use of zinc supplementation, so avoid high doses.
Zinc competes for absorption with other minerals such as iron. When high doses of zinc get consumed, absorption of iron and other vital minerals get decreased, resulting in deficiencies. The recommended daily intake of zinc is 11 mg and 8 mg for males and females aged 19 years and older. 75 mg is significantly higher than the daily recommended needs. Higher doses of zinc should be short-term and taken only when indicated.
We don’t want to create a new problem when trying to resolve another.
Practical takeaways and recommendations to maintain and support immune health:
- Practice good hygiene, such as hand washing.
- Aim to get enough good quality sleep.
- Manage physical and psychological stress.
- Eat a well-balanced diet – simple I know, but consumption of protein, carbohydrates from a variety of fruits, vegetables, and whole grains, and healthy fats with an emphasis on omega-3s can ensure that various nutrient needs are satisfied. Nutrition-wise, this is the most impactful!
- Make sure to consume enough calories to meet your demands and hit your total protein needs daily.
- If you are making weight or body composition changes when there are “risk factors” for infection, avoid drastic calorie reductions, and ensure protein intake to your needs — AVOID CRASH DIETING.
- Consume >50% of your daily energy intake from carbohydrates.
- 1-2 cold water fish meals per week (3 for the price of 1 – protein, vitamin D, and EPA & DHA!) or supplementation of 2-3 g of EPA + DHA.
- Consider vitamin D supplements between 1,000-4,000 IU D3 per day depending on the season (summer versus winter), skin color, and UVB or sun exposure.
- Consider increasing vitamin C intake to 100-200 mg + when the increased likelihood of infection, such as during travel, winter months, or sick people’s exposure.
- After the onset of a common cold, within 24 hours of experiencing symptoms, dissolve zinc lozenges (containing 75 mg of elemental zinc per day).
References
- Walsh, N. (2019). Nutrition and athlete immune health: new perspectives on an old paradigm. Sports Medicine, 49(Suppl 2): S153-S168.
- Woodward, B. (1998). Protein, calories, and immune defenses. Nutrition Review, 56(S84-S92).
- Drew, M et al. (2017). A multifactorial evaluation of illness risk factors in athletes preparing for the summer olympic games. Journal of Science and Medicine in Sport, 20,745-750.
- Peake JM, Neubauer O, Walsh NP, et al. (2017). Recovery of the immune system after exercise. Journal of Applied Physiology, 122(5):1077–87.
- Gleeson, M, Nieman, D, Peterson, K. (2004). Exercise, nutrition, and immune function. Journal of Sport Science, 22, 115-125.
- Carswell AT, Oliver SJ, Wentz LM, et al. (2018). Influence of vitamin D supplementation by sunlight or oral D3 on exercise performance. Medicine and Sciences in Sports and Exercise, 50(12).
- Owens, DJ. (2017). Efficacy of high-dose vitamin d supplements for elite athletes. Medicine and Science in Sports, and Exercise, 49, 349-356.
- Owens, DJ, Allison, R, & Close, G. (2018). Vitamin D and the athlete: current perspectives and new challenges. Sports Medicine, https://doi.org/10.1007/s40279-017-0841-9.
- Hao Q, Dong BR, Wu T. (2015). Probiotics for preventing acute upper respiratory tract infections.Cochrane Database Systematic Review.
- Cox AJ, Pyne DB, Saunders PU, et al. (2010). Oral administration of the probiotic lactobacillus fermentum vri-003 and mucosal immunity in endurance athletes. British Journal of Sports Medicine, 44(4),222–6.
- Carr, AC, & Maggini, S. (2017). Vitamin C and immune function. Nutrients, 9, 1211-1236.
- Hemil. H. (2017). Zinc lozenges and the common cold: a meta-analysis comparing zinc acetate and zinc gluconate, and the role of zinc dosage. JRSM Open, 8(5):2054270417694291.